FinDBest IVF is a global B2B platform that connects manufacturers of fertility and reproductive health devices with IVF-specialist distributors in over 150 countries. We simplify global expansion, regulatory pathway planning, and distributor onboarding.
Each year, the European Society of Human Reproduction and Embryology (ESHRE) Congress reveals not just clinical updates, but also clear signals about where the IVF market is heading. In 2025, Circular Communications compiled a focused commercial and product roadmap briefing from the event, kindly shared recently by Dr. Georg Griesinger on Linkedin. What follows is a practical breakdown of their insights—designed for medical device manufacturers and clinical users who need to make fast, evidence-based business and product decisions:

The Six Shifts Reshaping IVF
The IVF landscape in 2025 is not simply evolving—it is undergoing structural change. Six key forces are reshaping how medical devices are adopted, evaluated, and purchased. Manufacturers who adapt early will find more predictable paths to market. Those who do not risk falling behind as clinics tighten their criteria.
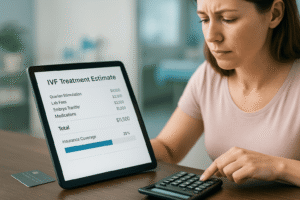
Cost pressures are now the central constraint. IVF remains financially inaccessible for large segments of the population. In many countries, patients are still paying out of pocket. The result is a growing preference for solutions designed around total cost of ownership (TCO). That means not just upfront purchasing price/cost, but reusability, reliability, throughput, maintenance needs, and training time. Products that align with capital expenditure (CAPEX) models and flexible subscriptions—especially those matched to clinic cash flow—are more likely to be adopted.
Growth in mature markets has flatlined. In many high-income countries, the number of IVF cycles per capita has plateaued. For manufacturers, that means growth must now come from share gain or geographic expansion, particularly into fast-growing regions like Southeast Asia, the Middle East and North Africa (MENA), and Latin America. But entering these markets successfully requires localizing value propositions and working with distributors who understand IVF workflows and regulatory constraints.
Legal and ethical oversight is tightening. Questions about embryo selection, long-term storage, and artificial intelligence (AI) in diagnostics are under increased scrutiny. For manufacturers, this raises the bar on traceability, audit readiness, and labeling compliance. Products now need to include support for standard operating procedures (SOPs), as well as detailed logging and audit trails. These are no longer differentiators—they are minimum requirements.
Patient experience has become a key decision factor. Clinics are under pressure to not only deliver outcomes but also reduce the emotional and cognitive burden on patients. Devices that simplify communication, reduce the number of steps in a procedure, and help patients understand “what’s next” are increasingly favored. Clear interfaces, intuitive indicators, and minimal user intervention all contribute to better adoption.
Clinic consolidation is shifting how buying decisions are made. Independent clinics are being replaced or absorbed by multi-site groups (Eg. US Fertility or IVIRMA, owned by KKR). These groups prioritize enterprise-style purchasing: standardized protocols, centralized training, measurable return on investment (ROI), and clear service levels. Manufacturers that can offer SOP kits, multi-site onboarding, and enterprise-level value metrics will have a distinct advantage.
Technology alone no longer drives differentiation. Automation, AI, microfluidics, smart incubation systems, and digital integration are becoming standard. The key to winning adoption now lies in reproducibility, data quality, interoperability, and auditability—not just product specifications. Clinics expect devices that integrate easily with their digital systems and produce consistent results across different settings.
Each of these shifts presents a challenge, but also a roadmap. Cost, regulation, technology, and buyer behavior are all converging toward a more structured and evidence-driven IVF market. Manufacturers who address these realities in their design, pricing, and commercial execution will be best positioned to scale.
Clinical and Technological Frontiers Highlighted at ESHRE 2025
Beyond the market dynamics, ESHRE 2025 spotlighted several areas of clinical innovation that are directly shaping device and diagnostics development. These themes are not theoretical—they are influencing purchasing, adoption, and regulatory expectations now.
Ovarian stimulation protocols are being rethought. As clinics aim for personalization and patient comfort, the need for smarter diagnostics and more flexible drug delivery systems is growing. Biomarkers that can predict ovarian reserve and treatment response are informing stimulation protocols, making room for devices that adapt to individual profiles. At the same time, there is a clear trend toward mild stimulation protocols, which create demand for less-invasive monitoring tools and delivery systems that are intuitive, reliable, and easy to train on. The ongoing refinement of protocols using gonadotropin-releasing hormone (GnRH) antagonists reinforces the need for workflow-agnostic solutions—those that can fit into varying cycles without adding complexity.
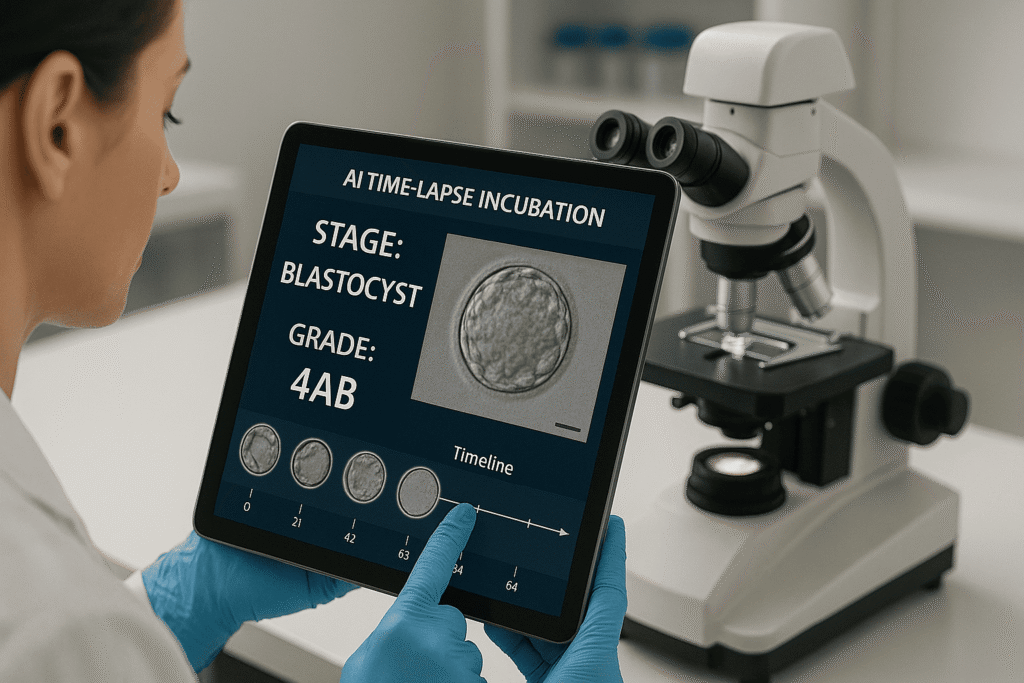
Embryo selection is moving well beyond morphology. Objective, evidence-backed methods are replacing subjective scoring. One major area of interest is AI-supported time-lapse imaging, which offers the potential to assess embryo viability in a more standardized and reproducible way. However, clinics are demanding validated tools—classified appropriately as software as a medical device (SaMD), with integration capabilities and clean clinical evidence. In parallel, non-invasive preimplantation genetic testing (niPGT) is gaining momentum. Media capable of capturing cell-free DNA (cfDNA), paired with ultra-sensitive genetic testing platforms, could redefine embryo selection workflows. This is not a future trend—it’s a present R&D priority. Manufacturers need to plan both the evidence and regulatory strategy from the outset. Metabolomics and biomarker analysis of culture media are also being explored, particularly where kits can offer clear utility and fit easily into existing lab infrastructure.

Implantation remains a key bottleneck. Even with viable embryos, successful transfer remains challenging. There is growing interest in non-invasive endometrial diagnostics that can assess uterine receptivity without disrupting workflow. The market demands tools that are specific, reproducible, and easy to use. Meanwhile, catheter design continues to influence both outcomes and patient experience. Ergonomics, atraumatic placement, and consistent delivery are still core drivers of successful transfers. While less discussed in marketing, this area remains a top priority for clinical users and therefore deserves more innovation attention.
Taken together, these frontiers point toward a product development path that favors integration over novelty, reproducibility over experimentation, and real-world usability over theoretical performance. It is not just what your device does—it is how it fits into the day-to-day life of clinics under pressure.

Regulatory and Market Access: Build It In, Not On
Global regulatory expectations are rising, and shortcuts are closing. Product teams can no longer afford to treat compliance as a post-development task. It must be embedded from Day 0.
For software and AI-based tools, classification is tightening across the United States, European Union, and China. This means developers must create full validation plans early, align endpoints with regulatory expectations, and document cybersecurity and data governance practices before launch. Post-market surveillance and post-market clinical follow-up are not optional; they need to be built into the development process.
Culture media and reagent products are under increased scrutiny from regulations like the European Union’s Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR). Manufacturers must establish robust quality systems, ensure all labeling is complete and language-appropriate, and be ready to implement unique device identification requirements in every target market.
For connected lab devices, regulatory bodies expect more than just functionality. They now require detailed documentation of data interoperability, security protocols, and integration capabilities. Manufacturers should design clean application programming interfaces (APIs) and seamless connectors for hospital and laboratory data systems to make compliance easier—not harder—for clinics.
A practical checklist for manufacturers:
- Confirm software classification and plan validation early for each market.
- Create templates for traceability, labeling, audit logs, and PMS/PMCF.
- Implement cybersecurity and data protection frameworks from Day 0.
- Ensure unique device identification (UDI) compliance for each geography.
- Offer clear integration documents for lab systems (no assumptions).

Strategic Focus Areas for IVF Device and Diagnostics Manufacturers
- Balance cost and innovation
Demonstrate lower total cost of ownership through real-world data. Show how your product reduces maintenance, training time, or consumable use. - Support with evidence, not claims
Build prospective, multi-site clinical studies. Prepare audit-ready documentation: instructions for use, labeling, traceability, and surveillance templates. - Integrate digital and physical
Provide open, secure APIs. Ensure fast and simple onboarding for embryologists and nurses. Focus on reducing clicks, errors, and delays. - Refine embryo selection strategy
Align product claims with validated inputs—whether AI models, cfDNA media, or metabolomic markers. Monitor data drift and revalidate regularly. - Improve uterine receptivity and transfer tools
Support claims with performance data (e.g. time to placement, consistency). Offer quick training modules to accelerate adoption. - Embed regulatory design
Maintain a live matrix of requirements per SKU and market. Don’t delay planning for UDI, cybersecurity, PMS/PMCF. - Sell to enterprise buyers
Offer group-level SOP kits, ROI calculators, and centralized onboarding. Provide remote diagnostics and clear SLAs to reduce downtime. - Speed up market entry through smarter distribution
Use IVF-experienced distributors with proven regulatory capabilities. Shorten time to first order by removing the guesswork.
Key Takeaways
- Total cost of ownership is now the key metric—design around it.
- Patient workflows and clinic processes must be simplified.
- Reproducibility and integration matter more than specs.
- Plan evidence generation around the claims you want to make.
- Prepare for audits with full traceability and post-market tools.
- Offer group-ready commercial packages for multi-site chains.
- Match each market with a localized regulatory strategy.
- Choose distributors who understand both IVF and compliance.
FinDBest IVF: Your Partner in Global Expansion
These insights from ESHRE 2025, as compiled by Circular Communications, offer a compelling glimpse into the future of fertility treatment. For medical device manufacturers, these trends are direct signals for where to focus R&D, innovation, and market entry efforts.
At FinDBest IVF, we specialize in helping medical device manufacturers navigate the complex global regulatory landscape. Whether you’re developing cutting-edge AI for embryo selection, next-generation culture media, or advanced cryopreservation devices, we can help you:
- Find regulatory-savvy distributors and license holders.
- Identify partners who understand country-specific timelines and dossier formats.
- Expand globally, faster — with fewer surprises.
Credits
- Original, full report by Circular Communications
- Shared on Linkedin by Dr. Georg Griesinger